159 North 3rd Street
Macclenny, Florida 32063
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.

Toenail fungus, medically known as onychomycosis, is a condition that affects countless individuals, causing nails to become discolored, brittle, and thickened. Traditional treatment methods, such as oral medications or topical ointments, often yield mixed results and can take months to show improvement. This is where laser therapy, a relatively new approach, comes into play. Laser therapy for toenail fungus, also referred to as laser mycotic nail treatment, involves the use of a concentrated beam of light to target and destroy the fungal organisms that are infecting the nail. The laser's energy penetrates the nail, without causing harm to the surrounding tissue, to eliminate the fungus at its source. This innovative approach boasts several advantages, including minimal discomfort, no need for anesthesia, and typically shorter treatment times compared with traditional methods. However, it is important to note that laser therapy is not a guaranteed cure and may require multiple sessions for the best results. While promising, its effectiveness varies from person to person. If you have toenail fungus, it is suggested that you visit a podiatrist who can determine if laser therapy is correct for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with Dr. John L. Coleman from Florida. Our doctor will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.

Flat feet, medically known as pes planus, is a common condition where the arch of the foot is abnormally low or nonexistent, causing the entire sole to touch the ground when standing. This can be due to various factors, such as genetics, obesity, pregnancy, or repetitive high-impact activities. While some people with flat feet experience no discomfort, others may develop symptoms that affect their daily lives. Flat feet can originate in childhood, where the arch has not yet developed, and may persist into adulthood. Over time, the wear and tear on the posterior tibial tendon can lead to the arch collapsing, resulting in overpronation. Ankles and knees can also be affected, as flat feet may cause the ankles to turn inward, leading to alignment issues in the legs. Symptoms can range from difficulty standing on tiptoe to knee and back pain, arch strain, and swelling along the inside of the ankle. When it comes to treatment, a range of options can help alleviate the discomfort associated with flat feet. Special shoes with strong heel counters, steel or carbon fiber shanks, and medial postings can assist in alignment. Custom-designed arch supports, molded to your foot's unique contours, are often recommended. Stretching exercises for a shortened Achilles tendon may also prove beneficial. For help in dealing with flat feet, it is suggested that you make an appointment with a podiatrist to determine the best course of action for your specific needs.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. John L. Coleman from Florida. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.

Athlete's foot, a common fungal infection, can cause discomfort and frustration for those affected. The symptoms often include itching, burning, and stinging sensations in the affected areas, generally between the toes or on the soles of the feet. Skin peeling, blistering, and dryness may also occur. This condition is primarily caused by various types of fungi, thriving in warm, damp environments such as locker rooms, swimming pools, and shared showers. Direct contact with the fungi through contaminated surfaces or by sharing shoes, towels, or socks can facilitate its spread. Additionally, individuals with sweaty feet or those who wear tight, closed toe shoes for extended periods are at higher risk. Maintaining proper foot hygiene, wearing breathable footwear, and keeping feet dry can aid in prevention and mitigate the symptoms of athlete's foot. Athlete’s foot is treated by a podiatrist, and it is suggested that you visit this type of doctor who can effectively treat this condition.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. John L. Coleman from Florida. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
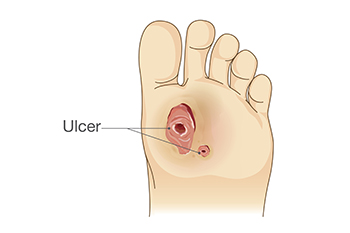
A foot ulcer is defined as any break in the skin. It is the most common type of diabetic foot wound and can lead to loss of functioning and severe complications. These foot wounds often result from factors such as poor blood sugar control, diabetic peripheral neuropathy, and abnormal foot mechanics due to deformities. Diabetic peripheral neuropathy, a side effect of diabetes, can also lead to a loss of protective sensation in the feet, making early injury detection challenging. The assessment of the diabetic foot involves a comprehensive foot and body examination. This can consist of assessing risk factors, undergoing a dermatologic and musculoskeletal evaluation, and having neurologic tests that can determine the degree of sensation. Treatment of diabetic foot ulcers includes debridement, wound culturing, and wound dressings. Additionally, it is important to monitor glycemic control and infection control. Their prevention and management are essential to improve the patient’s quality of life. If you have diabetes and have developed a foot wound or any other foot condition, it is strongly suggested that you make an appointment with a podiatrist who can evaluate your situation, and receive the appropriate treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. John L. Coleman from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.