159 North 3rd Street
Macclenny, Florida 32063


Foot stress fractures are common injuries that can significantly impact daily life and physical activities. It's essential to understand the basics of these fractures to prevent and manage them effectively. Stress fractures occur due to repetitive stress on the bones, often seen in athletes and runners, especially those who suddenly increase their activity levels. They are tiny cracks in the bone that can be difficult to detect initially, as symptoms may start mild and gradually worsen. Common signs include localized pain, swelling, and tenderness in the affected area. Resting and elevating the affected foot is crucial in the early stages of managing a stress fracture. Seeking prompt medical attention and avoiding weight-bearing activities can prevent further damage. Wearing proper footwear, implementing gradual exercise progression, and incorporating rest days into the routine are essential preventive measures. Understanding foot stress fractures empowers individuals to take proactive steps in maintaining foot health and avoiding potential complications. If you have a foot stress fracture, it is suggested that you speak to a podiatrist who can effectively treat this condition.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. John L. Coleman from Florida. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.

Your feet are your constant companions, carrying you through life's journey. When injuries occur, proper wound care is vital to ensure a speedy recovery and prevent complications. The following are steps that can be taken for proper wound care. Begin by washing your hands thoroughly with soap and water to avoid introducing bacteria into the wound. Gently cleanse the affected area with mild soap and warm water, patting it dry with a clean towel. Bleeding can be controlled by applying gentle pressure with a clean cloth or sterile gauze. Using an antiseptic solution or ointment can help to disinfect the wound and minimize the risk of infection. This can be followed by applying an adhesive bandage or sterile dressing to shield the wound from dirt and friction. Change the dressing regularly and keep an eye on any signs of infection, such as increased redness, swelling, or discharge. By following these simple wound care steps, you can safeguard the health of your feet. If the bleeding persists or the wound is deep, it is suggested to seek prompt medical attention from a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. John L. Coleman from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.

Hammertoe can be uncomfortable and unsightly. It is a noticeable foot condition that causes the second and third toes to bend upward at the middle joint. These toes are often difficult to straighten out, and can become painful. Additionally, blisters and corns may form on top of the affected toes where they meet the shoe, and wearing shoes may be uncomfortable. A common cause of hammertoe comes from wearing shoes that are too tight, with inadequate room for the toes to move freely in. A proper diagnosis consists of having a physical examination performed, followed by beginning the correct treatment. Toes may be splinted to keep them straight, and specific toe stretches can be performed. This may be effective in keeping the toes as flexible as possible. If you have developed hammertoe, it is strongly suggested that you are under the care of a podiatrist who can provide you with treatment options that are best for you.
Hammertoes can be a painful condition to live with. For more information, contact Dr. John L. Coleman of Florida. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
Risk Factors
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.

Orthotics are insoles that are worn in the shoes to provide additional support for the feet. They are used for different reasons, including overall foot health, abnormal foot structure, and various foot ailments. There are several kinds of orthotics to choose from. Orthotics that are prescribed by a podiatrist are designed to fit and correct an individual's unique foot and specific condition. They are made by taking an impression of the feet and can be successful in treating plantar fasciitis, flat feet, or heel spurs. Mass-produced inserts are referred to as prefabricated orthotics, and can fit a large range of foot types. They can be purchased in a pharmacy, and are available in numerous sizes and arch types. People who have mild foot pain may benefit from over-the-counter insoles, which may provide temporary relief. If you have any type of foot pain, it is strongly suggested that you consult with a podiatrist who can help you to choose the right type of orthotics based on the cause of your foot pain.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. John L. Coleman from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
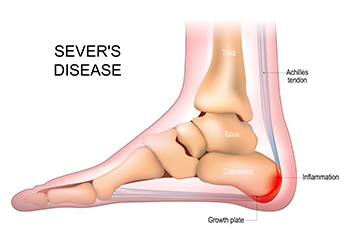
Heel pain in children may be a sign of Sever’s disease, which is a foot condition that affects physically active young children and teenagers. While it can cause severe pain and discomfort and is considered to be the most common cause of heel pain in children, it generally does not cause long-term damage. Sever's disease is defined as an inflamed growth plate in the heel. This can happen from excessive force or overuse, resulting in heel pain. This plate is necessary for shaping the heel bone, in addition to producing tissue for proper growth. Some types of activities that can contribute to developing Sever’s disease include running, jumping, or standing for extended periods of time. It can affect basketball or soccer players, and gymnasts may also feel the effects of Sever’s disease. Common symptoms that are associated with Sever's disease can consist of a swollen and reddened heel, and it can be difficult to walk. Mild relief may happen when the offending activity is temporarily stopped and the foot is frequently elevated. If your child has heel pain, it is strongly suggested that you consult with a podiatrist who can effectively diagnose and treat Sever's disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Dr. John L. Coleman from Florida. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.